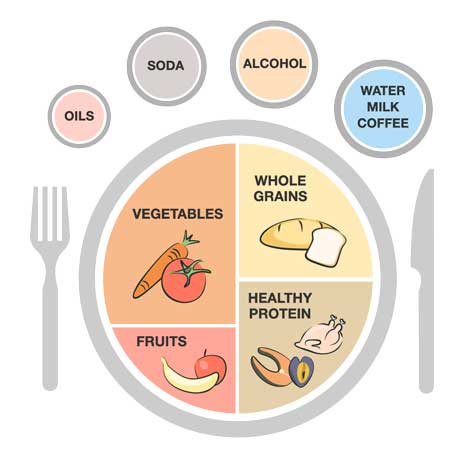
Non-pharmacologic Recommendations
- Obesity, dietary factors
- Excessive alcohol intake
- Metabolic syndrome, type 2 diabetes mellitus
- Hypertension
- Hyperlipidemia, modifiable risk factors for coronary artery disease or stroke
- Medications that induce hyperuricemia
- History of urolithiasis
- Chronic kidney, glomerular, or interstitial renal disease (e.g., analgesic nephropathy, polycystic kidney disease)
- In selected cases, potential genetic or acquired cause of uric acid overproduction (e.g., inborn error of purine metabolism or psoriasis, myeloproliferative, or lymphoproliferative disease, respectively)
- Lead intoxication
Fats and Oils
- Healthy Oils: Recommend healthy oils such as olive, canola, sunflower, coconut, soy, and corn.
- Bad Fats: Limit butter. Avoid trans fats.
- Good Fats: Healthy fats, including omega 3 fatty acids and unsaturated fats are recommended as part of a healthy, well-balanced diet.
Healthy Protein
- Limit: Limit sources of protein, especially red meats, the main source of purines (e.g., beef, pork, lamb). Avoid processed meats (e.g., bacon, cold cuts).
- Seafood: Tailor seafood intake. Seafood (tuna, dark fish, shrimp, lobster, scallops) is associated with a high risk of gout. Consuming heart-healthy fish (salmon, mackerel, herring, lake trout) is recommended as part of a healthy balanced diet.
- Poultry: Recommend a healthier source of protein and does not increase the risk of gout flares.
- Nuts and Legumes: (beans and lentils), despite their high purine content, are associated with lower risk of gout and are healthy dietary choices for gout patients.
Whole Grains
- Limit: refined grains (e.g., white rice, white bread).
- Eat whole grains, brown rice, whole-wheat bread, and whole-grain pasta.
- Fiber helps move waste (uric acid) through the digestive tract
Fruits
- Fruit: Recommend plenty of fruits of all colors. Daily fruit intake is recommended as part of a healthy, well-balanced diet. Make half the plate fruits and vegetables.
- Vitamin C: Recommend taking a vitamin C supplement, as it may be a useful option to prevent the development of gout in the first place.
- Cherry Juice: Intake of cherry products has been shown to reduce the risk of recurrent gouty flares.
Vegetables
- Vegetables: Recommend a variety of vegetables. Make half the plate vegetables and fruit as part of a healthy, well-balanced diet.
- Potatoes: Choose vegetables other than potatoes.
- Purines: Purine-rich vegetables (spinach, mushrooms, cauliflower), nuts and legumes (beans and lentils) are not associated with the risk of gout and are healthy dietary choices for gout patients.
Sugary Drinks
- Sodas: Eliminate sugar-sweetened beverages. In increased amounts, they are strongly associated with a higher risk of gout in men and women.
- Fructose: Fruit juices that are high in fructose increase sUA levels and the risk of gout.
- High Fructose Corn Syrup: HFCS intake has been linked to increased insulin resistance, a positive energy balance, weight gain, obesity, type 2 diabetes, an increased risk of certain cancers, and symptomatic gallstone disease.
Alcohol
- Beer and Liquor: Recommend limiting alcoholic beverages, particularly beer and liquor. Beer and liquor break down into uric acid and thus increase the risk of gouty flares
- Wine: In moderation, wine has a protective effect against cardiovascular disease.
- Limit: Limit to one to two drinks per day for men. Limit one drink per day for women. Recommend avoiding alcohol during flares and for uncontrolled gout.
Water
- Water: Recommend drinking lots of water. Water is the best option for beverage choice.
- Low-fat Milk: Low-fat dairy products have been shown to lower the risk of gout flares.
- Tea and Coffee: Use little or no sugar in your tea or coffee. Drinking caffeinated beverages in limited amounts has also been shown to lower the risk of gout flares.
- Niacin for management of hyperlipidemia
- Thiazide and loop diuretic for hypertension
- Calcineurin inhibition with cyclosporine or tacrolimus, if not essential for immune suppression (discuss with transplant team)
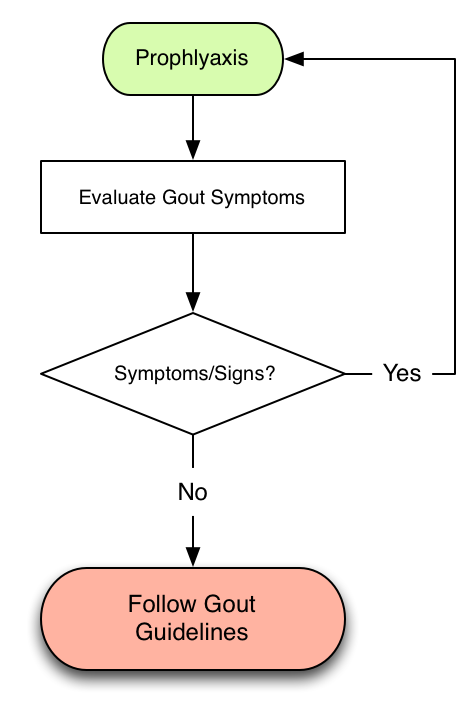
Guidance for Management of Acute and Chronic Gout
Adapted from the 2020 American College of Rheumatology Gout Guidelines for the Management of Gout
Indications for Pharmacologic Urate Lowering Therapy (ULT)
Strongly recommended for gout patients with any of the following:
- ≥1 subcutaneous tophi
- Evidence of radiographic damage (any modality) attributable to gout
- Frequent gout flares, with frequent being defined as ≥2 annually
Conditionally recommended for
- Patients who have previously experienced >1 flare but have infrequent flares (>2/year)
Conditionally recommended against
- In patients with asymptomatic hyperuricemia
- In patients with gout experiencing their first gout flare (*See exceptions below)
*However, initiating ULT is conditionally recommended for patients who are experiencing their first gout flare in the setting of any of the following:
- comorbid moderate-to-severe CKD (stage ≥3)
- SU concentration >9 mg/dl
- urolithiasis
Recommendations for choice of initial ULT for patients with gout
Strongly recommended
- Treatment with allopurinol as the preferred first-line agent over all other ULTs for all patients, including those with moderate- to- severe CKD (stage ≥3
- The choice of either allopurinol or febuxostat over probenecid for patients with moderate-to-severe CKD (stage ≥3)
- Starting treatment with low-dose allopurinol (≤100 mg/day and lower in patients with CKD [stage ≥3]) and febuxostat (≤40 mg/day) with subsequent dose titration over starting at a higher dose
- Administering concomitant anti-inflammatory prophylaxis therapy (e.g., colchicine, nonsteroidal antiinflammatory drugs [NSAIDs], prednisone/prednisolone) over no anti-inflammatory prophylaxis therapy
- Continuing concomitant anti-inflammatory prophylaxis therapy for 3–6 months over <3 months, with ongoing evaluation and continued prophylaxis as needed if the patient continues to experience gout flares
Strongly recommend against
- Pegloticase as a first-line therapy
Conditionally recommended
- Starting treatment with low-dose probenecid (500 mg once to twice daily) with subsequent dose titration over starting at a higher dose
Timing of ULT initiation
Strongly recommended for all patients receiving ULT:
- A treat-to-target management strategy that includes ULT dose titration and subsequent dosing guided by serial SU measurements to achieve a target SU, over a fixed-dose ULT strategy
- Achieving and maintaining an SU target of <6 mg/dl over the use of no target
Conditionally recommended
- Starting ULT during the gout flare over starting ULT after the gout flare has resolved, when ULT is indicated while the patient is experiencing a gout flare
- Delivery of an augmented protocol of ULT dose management by nonphysician providers to optimize the treat-to-target strategy that includes patient education, shared decision-making, and treat-to-target protocol
Duration of ULT
Conditionally recommended
- Continuing ULT indefinitely over stopping ULT
Recommendations for patients receiving ULT medications
Allopurinol
Strongly recommended
- Starting allopurinol in daily doses of ≤100 mg (and lower doses in patients with CKD) over starting at a higher dose
Conditionally recommended
- Testing for the HLA–B*5801 allele prior to starting allopurinol for patients of Southeast Asian descent (e.g., Han Chinese, Korean, Thai) and for African American patients, over not testing for the HLA–B*5801 allele
- Allopurinol desensitization for patients with a prior allergic response to allopurinol who cannot be treated with other oral ULT agents.
Conditionally recommended against
- Universal testing for the HLA–B*5801 allele prior to starting allopurinol in patients of non-Southeast Asian descent or African American patients
Febuxostat
Conditionally recommended
- Switching to an alternative oral ULT agent, if available and consistent with other recommendations, for patients taking febuxostat with a history of CVD or a new CVD-related event
Uricosurics
Conditionally recommended against
- Checking urinary uric acid prior to starting any uricosuric treatment
- Akalinizing urine
When to consider changing ULT strategy
Conditionally recommended
- Switching to a second XOI over adding a uricosuric agent for patients taking their first XOI, who have persistently high SU concentrations (>6 mg/dl) despite maximum-tolerated or FDA-indicated XOI dose, and who have continued frequent gout flares (>2 flares/year) OR who have nonresolving subcutaneous tophi
Strongly recommended
- Switching to pegloticase over continuing current ULT for patients with gout for whom XOI treatment, uricosurics, and other interventions have failed to achieve the SU target, and who continue to have frequent gout flares (≥2 flares/year) OR who have nonresolving subcutaneous tophi
Strongly recommend against
- Switching to pegloticase over continuing current ULT is strongly recommended against for patients with gout for whom XOI treatment, uricosurics, and other interventions have failed to achieve the SU target, but who have infrequent gout flares (<2 flares/year) AND no tophi
Gout flare management
Strongly recommended
- Using colchicine, NSAIDs, or glucocorticoids (oral, intraarticular, or intramuscular) as appropriate first-line therapy for gout flares over IL-1 inhibitors or adrenocorticotropic hormone (ACTH)
- Given similar efficacy and a lower risk of adverse effects, low-dose colchicine over high dose colchicine is strongly recommended when colchicine is the chosen agent
- Treatment with glucocorticoids (intramuscular, intravenous, or intraarticular) over IL-1 inhibitors or ACTH for patients who are unable to take oral medications
Conditionally recommended
- Using topical ice as an adjuvant treatment over no adjuvant treatment
- Using an IL-1 inhibitor over no therapy (beyond supportive/analgesic treatment) for patients experiencing a gout flare for whom the above antiinflammatory therapies are either ineffective, poorly tolerated, or contraindicated
Management of lifestyle factors
Conditionally recommended
- Limiting alcohol intake, regardless of disease activity
- Limiting purine intake, regardless of disease activity
- Limiting high-fructose corn syrup intake, regardless of disease activity
- Using a weight loss program (no specific program endorsed) for those patients with gout who are overweight/obese, regardless of disease activity
Conditionally recommend against
- Adding vitamin C supplementation, regardless of disease activity
Management of concurrent medications
Conditionally recommended
- Switching hydrochlorothiazide to an alternate antihypertensive when feasible, regardless of disease activity
- Choosing losartan preferentially as an antihypertensive agent when feasible, regardless of disease activity
Conditionally recommend against
- Stopping low-dose aspirin (for patients taking this medication for appropriate indications), regardless of disease activity
- Adding or switching cholesterol lowering agents to fenofibrate, regardless of disease activity
Treatment to Target Serum Urate
Lower serum urate to less than 6mg/dL to improve gout signs and symptoms. In tophaceous gout, the goal is less than 5 mg/dL.